ATTENTION: Intense pain radiating down the leg is usually a RED FLAG and should be checked out by a professional. If you have these symptoms, stop reading this and continue reading it in the waiting room of a qualified healthcare practitioner.
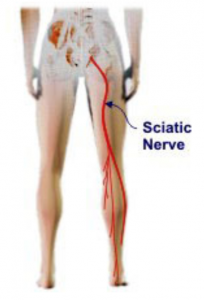
The sciatic nerve is a large nerve that forms out of the lower end of the spinal cord, travels down the back of the thigh, and branches off into smaller nerves as it continues to the lower leg and toes. Nerves travel in and out of muscle tissue, providing motor output and sensory input for various parts of the body. Imagine a piece of spaghetti (or in the case of the sciatic nerve, a garden hose!) traveling in, out, around, and through muscle tissue. Although there are many other nerves that are susceptible to irritable neural tension (femoral nerve, median nerve, ulnar nerve, and radial nerve to name but a few), this article will focus primarily on the sciatic nerve.
https://www.lancula.com/blogs/articles/the-cause-of-sciatic-nerve-pain
How Is It Placed Under Tension?
Nerves can have physical tensile connections to the neck and head because nerves, such as the sciatic nerve, originate in the spinal cord, which originates in the brainstem. This means that neural tension can be greatly affected by the position of the neck and head.
In the clinic, there is a provocative test to assess neural tension called the Slump Test. Reliability and validity aside, the test tensions the sciatic nerve (and other structures in the area) from both ends. The patient is asked to bring the chin to the chest, look downward, slouch forward at the spine, kick one leg out straight, and point the toes back toward the head. In other words, the patient gets into a position of cervical flexion, thoracic flexion, lumbar flexion (posterior pelvic tilt), hip flexion, knee extension, and ankle dorsiflexion. Keep in mind that the test position is meant to be provocative. Once in the test position, the patient will likely report tightness or a “stretching” feeling in the buttock and back of the thigh. The clinician then puts one end of the system on slack by asking the patient to lift the head up.
If the patient reports less tightness in the back of the thigh just by raising the head, the clinician can usually be sure that the tension is likely neural tension as opposed to muscular. If the tightness were from something like the hamstrings, lifting the head would have NO effect because the hamstrings have no connection to the head and neck. Understanding the difference between muscle stretch and neural stretch is key.
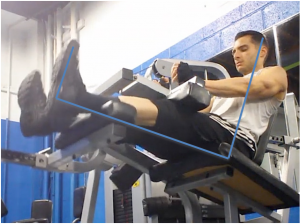
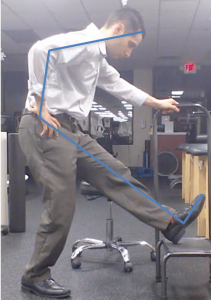
This picture is going to be used as a reference as the position of maximum sciatic tension. My blue line roughly traces the path of the sciatic nerve here and on the pictures below.
https://learnmuscles.com/blog/2017/08/14/special-orthopedic-assessment-tests-space-occupying-conditions-slump-test/
Why Is This Important? Should We Fear That Position?
As mentioned above, the Slump Test position is meant to be provocativesoif there are underlying or recurrent sciatic problems, it would probably serve us (and our nerves) well to avoid that position. I don’t want you to fearthis position and create a “nocebo effect.” The provocative test position willanatomically place tension on the sciatic nerve, but that doesn’tmean it is necessarily dangerous.
Is squatting 500lbs dangerous to someone who has spent a lifetime progressively training the squat? No. Can it be dangerous to someone who’s never stepped under a loaded barbell? Yup. We’re all different and our bodies are capable of different things, so keep that in mind. The position may not be a problem for you individually, but if there were simple ways to alter our form to reduce neural tension without compromising training, why wouldn’t we do it?
I want to once again make it very clear that I am not saying that these positions are somehow dangerous or that they should be avoided. A certain degree of neural tension is normal, and our nerves are meant to slide, glide, and stretch with movement. What I amsaying is that ifyou happen to have nerve pain already, you may want to avoid these positions.
Let’s Use The Seated Hamstring Curl As An Example (pictures below)
When performing the seated hamstring curl, be aware of the position of your head, neck, and upper back. Cervical, thoracic, lumbar, and hip flexion combined with knee extension and dorsiflexion is the position of maximum sciatic tension and is the exact position we assume, under load, when we perform the seated hamstring curl incorrectly. Keeping the upper body and neck upright against the back pad will ensure that the stretch we feel during the eccentric portion of the exercise is in fact muscular and not neural. The stretch in the back of the thigh at the start of the exercise will likely feel less intense when the upper body is upright and pinned against the back pad compared to when it is slumped and flexed forward. Remember, the hamstrings do not connect to the neck and upper back, but the sciatic nerve does. So, keeping the upper body straight or flexed will not increase or decrease the stretch on the hamstrings, but it will change the tension on the sciatic nerve. By sitting back and avoiding slouching forward, we are maintaining the stretch on the hamstrings while decreasing the stretch on the sciatic nerve (and Bingo was his name-o!).
A Message to Clinicians And Patients Alike…Keep It Simple When Warranted
Healthcare providers tend to overcomplicate things, especially physical therapists. I’m not sure if it makes us feel smarter or more relevant, but sometimes ditching the flashy terms and treatments and keeping it simple is the way to go. If you go to five different providers with complaints of sciatic-type pain, I can almost guarantee you will get five different causes and five different treatment options. You will likely be viewed like a malfunctioning car that needs adjusting, stretching, myofascial releasing, neuromuscular re-educating, and of course bird dogs and planks. While those things mayhave their place at times, I think the simple solutions are often overlooked. Patients are not machines and we are not mechanics.
For a moment, imagine pain as a moving car. How do we stop it? FIRST, we take our foot off the gas. THEN we hit the brakes. The order here is key. Stop the stimulus that is causing the car to accelerate and thenslow the car down with the brakes. No matter how new and shiny the brakes are or how cutting edge your technique is for hitting the brakes, you’ll meet resistance if you don’t first take your foot off the gas.
Sometimes coping with pain has less to do with adding flashy treatment systems, injections, or medications and more to do with modifying what already exists. Not sure if he actually said this, but it has been said that when talking about the statue of David, Michelangelo (not the Ninja Turtle) said he started with a stone and simply chipped away everything that wasn’t David.
****Before We Go On****
As mentioned above, these exercises and positions are NOT “dangerous” by nature. Performing them in the following manner will likely place the sciatic nerve on stretch, but whether or not that is a bad thing will depend on the individual. It’s not black and white or “good” and “bad.”
From the pictures, it may seem like I am talking about “good” and “bad” posture or “good” and “bad” form, but that is not my intention. All I am trying to show here are positional changes that can impact neural tension. There probably are not “good” and “bad” postures anyway, but that’s a whole other discussion!
Common Examples
Seated Straight Leg Calf Press
No
Better
Leg Press
No
Better
Leg Extension
No
Better
Seated Hamstring Curl
No
Better
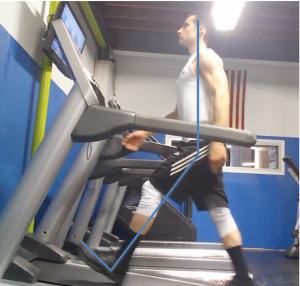
Incline Treadmill Walking
No
Better
Hamstring Stretch
No
Better
Driving
No
Better
To Wrap It Up
Like I said, there is NOTHING wrong or inherently dangerous about the positions mentioned in this article; however, if you aresuffering from sciatic-type symptoms, you may want to avoid them.
So, before blaming an unstable core, weak glutes, problematic SI joint, tight hip flexors, anterior pelvic tilt, hypomobile thoracic spine, a herniated disc, degenerative disc disease, leg length discrepancy, pelvic dysfunction, the Cookie Monster, or any other nebulous scary sounding “diagnosis,” try simple positional modifications to take your foot off the gas.
Simply put, the goal should be to stop provoking the painful stimulus, while maintaining a training effect. This allows Mother Nature to do her thing, so we can work our way back to the desired movement pattern through graded exposure to desensitize the system to the painful response. Jordan fades back, shoots, and THAT’S THE GAME! Nothing further, your honor…













Thanks. This article was really helpful. I think falling into some of those poor postures has been contributing to my sciatic symptoms.
Hey Michael! Thanks so much. I’m glad you found the article helpful! These positions can no doubt exacerbate sciatic symptoms, but remember that they aren’t inherently “bad.” If you are having sciatic-type symptoms, it can’t hurt to get it checked out. If you’ve seen a healthcare practitioner about it, then great! If not, it may be a good idea to consider. Either way, feel free to reach out with any questions! Thanks again!
This was super helpful. Thank you so much!!!!!!! 3dmj goats
Our pleasure!!!
Hi Nicholas. Not sure if this comment thread is still open but just wanted to say I have been struggling with sciatica for a few months now and think the exact exercises you use for reference in the article are those which have caused my pain. My physio has recommended not doing these exercises but I wondered if you feel resuming them at low loads with the posture modifications you suggest might actually help my recovery? Thanks in advance.
Hey Mike thanks for reaching out! Sorry to hear that you’ve been dealing with this for a few months. Great question about whether you should modify the movements or simply take them out of your program while the symptoms calm down. I’ve seen success with both approaches, but I’d say go with what your physio recommended since he/she has evaluated you and developed a treatment plan based on that evaluation. That being said, if you feel like your physio isn’t keeping your goals in mind or you two don’t quite see eye to eye, you can always seek out other opinions. Sometimes it’s not that someone is right or wrong in their approach, just different. I hope that helps! Feel free to reach out with any other questions! Nick@strengthtogetheronline.com
Thank you for the reply! I have taken the exercises out completely for about 8 weeks but feel that a gentle re-introduction feels like a sensible next step to getting back to somewhere near my pre-injury training. Thanks again.
Great!